News Item
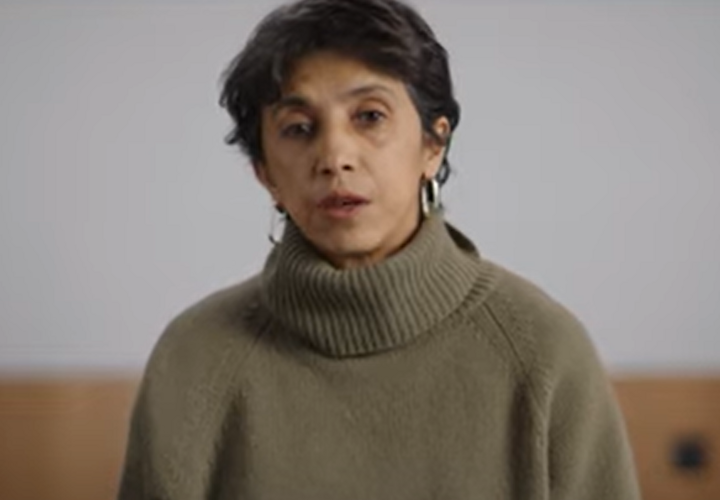
Pinelopi Koujianou Goldberg's research featured by the BBC: "Why female entrepreneurs are key to getting more women to work" … Pinelopi Koujianou Goldberg's research featured by the BBC: "Why female entrepreneurs are key to getting more women to work" In …
Relevance: 15.695752